Busting the Myths of Calcium for Bone Health
Calcium for bone health?
For decades now, calcium supplements – with or without vitamin D – have become the mainstay of advice to prevent bone loss – also called osteoporosis. Calcium supplements have also been recommended for many years to elderly people in order to help prevent fractures.
The ongoing advice over the years has been that adults need to take somewhere in the range of 1,200 milligrams a day in order to stave off fractures and bone loss in future years. Some advice has been more aggressive: Consuming between 2,000 to 3,000 milligrams of calcium per day.
And since the average Western diet will typically contain between 700 and 900 milligrams, this means ongoing advice for supplementing calcium at anywhere between 500 to 1,200 milligrams per day.
All this has led to a rate of as high as half of some populations – for example older women – taking calcium supplements in some Western countries.
Yet studies over the past five years have found that taking calcium supplements can have some adverse responses, including increased risk of heart disease and higher rates of kidney stones. Others have reported gastrointestinal symptoms from time to time.
Illustrating this cardiovascular risk, a 2011 meta-analysis study included over 44,000 older women who had either been taking calcium or started taking calcium at the beginning of the studies. This 2011 meta-analysis showed that taking calcium with or without vitamin D increased the risk of a heart attack by between 13 and 24 percent, depending upon when the calcium supplementation began. Taking calcium or calcium plus vitamin D also increased the risk of stroke by some 16 percent.
Other research has presented similar conclusions – regardless of whether vitamin D was included in the supplement.
This news has certainly quashed some of the advice regarding calcium, but only a little. The news simply added a caveat to supplementation. It was either bone loss or increase the risk of heart attack.
In this article
Doesn’t Calcium doesn’t prevent fractures?
The ongoing advice has partly continued because of the relative insistence by many that calcium supplementation prevents fractures. Is it true?
Certainly a number of studies have shown that calcium supplementation can reduce the rate of bone fractures. Most of these were large observational studies. The only problem is there has been something bending the results a little: Something called bias.
There are several types of bias in research. For example, publication bias is when those studies with greater results get published and those studies with not so much don’t. Other types of bias found in research include selection bias, intervention bias, and measurement bias. These various types of bias can interplay within a collection of studies as they are reviewed. And they can skew the results.
Finding bias among research can be done with a complicated statistical tests such as Egger’s test. I won’t bog you down with too many more details – as this is statistics. The bottom line is that medical research bias can be determined mathematically and the rules for the assessment of bias has been established in on a peer-reviewed basis from the respected Cochrane Handbook of meta-study research.
Multiple studies show calcium doesn’t prevent fractures
A late 2015 study found these types of bias exist in much of the calcium-bone fracture research. They applied the Cochrane Handbook assessments for bias and found that most of the studies that showed calcium reduced fractures were biased, and those with low bias showed clearly that calcium did not change the fracture rate.
The researchers, from the University of Auckland, conducted a meta-analysis that included 44 studies on calcium and bone fractures. These included many thousands of people. The studies tracked the intake of dietary calcium, milk or dairy consumption, and the rate of fractures among large populations of people.
The research found that most studies did not find that calcium supplementation reduced bone fractures. Those that did were tripped up with bias after applying Egger’s test.
But in those studies with no or minimum bias – which included over 44,000 people – calcium intake had no net effect upon bone fracture rates. And this is regardless of whether the calcium was combined with vitamin D or not.
This doesn’t mean that none of the low bias research showed benefit. The researchers only found one study – of frail elderly women in residential care – where supplementation reduced fracture rates. But these were of women who had diets grossly deficient in calcium. These women did show a reduction in fractures with calcium supplementation.
But the mass majority of trials, after bias was calculated out, showed calcium supplementation had no effect upon bone fractures.
The researchers concluded their findings:
“Overall, there is little evidence currently to suggest an association between calcium intake and fracture risk or that increasing calcium intake through dietary sources will alter risk. Although calcium supplements produced some small inconsistent reductions in fractures, the doses used of 500-1600 mg/day gave an average total daily calcium intake of 1780 mg/day (range 1230-2314 mg/day). This is considerably higher than the dietary calcium intake in the highest quarter or fifth in the prospective observational studies.”
But sustaining these levels of calcium can also be problematic, as I mentioned above. For example, in a study of more than 36,000 women, the risk of kidney stones among those taking the calcium increased by 17 percent. This study did not report on cardiovascular problems as others have.
What about calcium and bone loss?
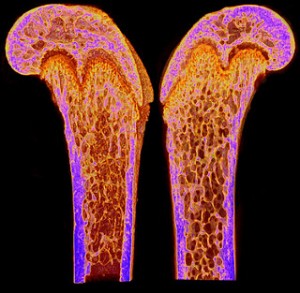
Bone mineral density is the technical phrase describing bone loss – or osteoporosis. When the bones lose mineral density as picked up by a bone density scan, this results in weaker, more brittle bones.
Despite their apparent rigidity, bones are metabolically active. Bone is composed of minerals (50-70%), an organic matrix (20-40%), water and lipid. Bone constantly remodels through bone resorption, mainly by ostoclasts and bone formation mainly by osteoblasts. As people age, bones may become brittle or osteoporotic when osteoclast activity exceeds osteoblast activity.
The assumption that calcium results in significant bone mineral density gain has been engrained into Western medicine for at least two decades. This assumption has also come partly as a result of publication bias – practitioners focusing on studies showing a greater benefit and not on others. But the meta-analysis results as all the studies are calculated are clear: The ability of calcium supplementation to increase bone mineral density is minimal at best.
In this meta-analysis – also published in the British Medical Journal – the researchers calculated results from 59 randomized and controlled studies. These studies followed those who took calcium and those who didn’t.
Some of the studies used calcium supplementation of greater than 500 milligrams per day. A greater number used more than 1,000 milligrams per day. Most of the studies did not include vitamin D, but some did.
Combined, the studies examined bone density and calcium supplementation in a total of 12,257 people. Of these supplementing or increasing calcium intake for a year or more resulted in a mere 0.6 to 1 percent increase in hip bone density, and a paltry 0.7 to 1.8 percent increase in bone mineral density of the lumbar spine and femoral neck. There was no net increase in bone density of the forearm in these studies.
When comparing calcium supplements to increasing calcium intake from dietary sources, the results were about the same.
Furthermore, the research found that continuing to take calcium did not offer increased bone density after the initial year. In other words, those taking the calcium for more than two years saw no further gains over those minor gains made in the first year.
The bias testing found that 19 of the studies had low bias, while 32 of the others had moderate or high risk of bias.
The evidence was strong enough for the researchers to state:
“In summary, increasing calcium intake from dietary sources increases bone mineral density by a similar amount to increases in bone mineral density from calcium supplements. In each case, the increases are small (1-2%) and non-progressive, with little further effect on bone mineral density after a year. Subgroup analyses do not suggest greater benefits of increasing calcium intake on bone mineral density in any subpopulation based on clinically relevant baseline characteristics. The small effects on bone mineral density are unlikely to translate into clinically meaningful reductions in fractures. Therefore, for most individuals concerned about their bone density, increasing calcium intake is unlikely to be beneficial.”
Calcium with or without vitamin D
The results of reviews for both of these issues – bone density and bone fracture – are the same even with calcium plus vitamin D, whether D2 or D3. Note that these did not address the body’s best form of vitamin D from sunlight (or sun lamps).
For example, a large clinical study from Ohio State University included 36,272 women. This study found that calcium plus vitamin D only increased the bone mineral density by an average of 1.06 percent. That is pretty tiny. Plus as mentioned above, the risk of kidney stones increased by 17 percent.
High calcium intake may actually be detrimental to bone health
There is also another issue about calcium to consider.
Dr. Mark Hegsted was a nutrition professor at Harvard for several decades. He was the administrator of the human nutrition unit at the Department of Agriculture for four years, and the principle designer of the first “Dietary Guidelines for Americans.” Dr. Hegsted was also a leading calcium researcher.
In a 1986 study published in the Journal of Nutrition, his team found that countries with higher dietary calcium intakes also had higher rates of hip fractures. The United States topped this list with the most hip fractures. Other high hip fracture countries included New Zealand and Sweden.
Dr. Hegsted concluded:
“Hip fractures are more frequent in populations where dairy products are commonly consumed and calcium intakes are relatively high.”
Is there another dietary issue related to bone loss?
In 2000., researchers from the University of California/San Francisco’s Department of Medicine and Clinical Research Center led by Dr. Lynda Frassetto conducted another analysis. They analyzed the hip fracture rates in women over 50 years old among 33 countries around the world, using 87 different surveys. They compared this with the per capita consumption of vegetable and animal foods from reports by the United Nations Food and Agriculture Organization.
The research revealed that the countries with the lowest rates of animal protein consumption – and greater levels of plant-based proteins – had the least hip fracture rates. Meanwhile, those countries with higher animal protein consumption also had higher rates of hip fractures.
The United States had the third highest rates of hip fractures per capita, behind Australia and New Zealand. All three countries have the highest levels of calcium consumption and high animal protein intake. The researchers added that this was:
“… a finding that suggests that bone integrity is compromised by endogenous acid production consequent to the metabolism of animal proteins.” They added that, “vegetable foods might provide a countervailing effect, because they are a rich source of base (bicarbonate) in the form of metabolizable organic anions, which can neutralize protein-derived acid and supply substrate (carbonate) for bone formation.”
After reviewing the details of these elements of diet, the researchers concluded:
“The findings suggest that the critical determinant of hip fracture risk in relation to the acid-base effects of diet is the net load of acid in the diet, when the intake of both acid and base precursors is considered. Moderation of animal food consumption and an increased ratio of vegetable/animal food consumption may confer a protective effect.”
They also stated:
“Our group has shown that contemporary net acid-producing diets do indeed characteristically produce a low-grade systemic metabolic acidosis in otherwise healthy adult subjects, and that the degree of acidosis increases with age, in relation to the normally occurring age-related decline in renal functional capacity.”
Dr. Frassetto and fellow University of California/San Francisco researchers continued to investigate the historical mineral composition in the diet together with osteoporosis in their clinical research. They concluded that in Western diets, potassium alkali salts (K-base) in the diet have been largely replaced by a sodium chloride (NaCl)-rich diet. The K-base potassium alkali salts are prominent among plant-based foods.
In other words, our salty diets have largely replaced the alkaline diets rich in alkaline salts, particularly potassium and magnesium.
Furthermore, the researchers found that administering NaCl (salt) increased urinary calcium excretion, and increased.
Their research also found that supplementation with potassium bicarbonate (KHCO3) “improved calcium and phosphorus balances, reduced bone resorption rates, improved nitrogen balance, and mitigated the normally occurring age-related decline in growth hormone secretion–all without restricting dietary NaCl.”
They also found that supplementing an alkalinizing salt of potassium (potassium citrate) together with NaCl (salt) prevented the salt from increasing urinary calcium excretion and bone resorption. Dr. Frassetto adds:
“Theoretically, we humans should be better adapted physiologically to the diet our ancestors were exposed to during millions of years of hominid evolution than to the diet we have been eating since the agricultural revolution a mere 10,000 years ago, and since industrialization only 200 years ago. Among the many health problems resulting from this mismatch between our genetically determined nutritional requirements and our current diet, some might be a consequence in part of the deficiency of potassium alkali salts (K-base), which are amply present in the plant foods that our ancestors ate in abundance, and the exchange of those salts for sodium chloride (NaCl), which has been incorporated copiously into the contemporary diet, which at the same time is meager in K-base-rich plant foods. Deficiency of K-base in the diet increases the net systemic acid load imposed by the diet. We know that clinically-recognized chronic metabolic acidosis has deleterious effects on the body, including growth retardation in children, decreased muscle and bone mass in adults, and kidney stone formation, and that correction of acidosis can ameliorate those conditions. Is it possible that a lifetime of eating diets that deliver evolutionarily superphysiologic loads of acid to the body contribute to the decrease in bone and muscle mass, and growth hormone secretion, which occur normally with age? That is, are contemporary humans suffering from the consequences of chronic, diet-induced low-grade systemic metabolic acidosis?
Earlier studies estimated dietary acid load from the amount of animal protein in the diet, inasmuch as protein metabolism yields sulfuric acid as an end-product. In cross-cultural epidemiologic studies, Abelow found that hip fracture incidence in older women correlated with animal protein intake, and they suggested a causal relation to the acid load from protein. Those studies did not consider the effect of potential sources of base in the diet. We considered that estimating the net acid load of the diet (i. e., acid minus base) would require considering also the intake of plant foods, many of which are rich sources of K-base, or more precisely base precursors, substances like organic anions that the body metabolizes to bicarbonate.
In following up the findings of Abelow et al., we found that plant food intake tended to be protective against hip fracture, and that hip fracture incidence among countries correlated inversely with the ratio of plant-to-animal food intake. These findings were confirmed in a more homogeneous population of white elderly women residents of the U.S. These findings support affirmative answers to the questions we asked above. Can we provide dietary guidelines for controlling dietary net acid loads to minimize or eliminate diet-induced and age-amplified chronic low-grade metabolic acidosis and its pathophysiological sequelae. We discuss the use of algorithms to predict the diet net acid and provide nutritionists and clinicians with relatively simple and reliable methods for determining and controlling the net acid load of the diet. A more difficult question is what level of acidosis is acceptable. We argue that any level of acidosis may be unacceptable from an evolutionarily perspective, and indeed, that a low-grade metabolic alkalosis may be the optimal acid-base state for humans.”
Dr. Hegsted stated in 2001 in the American Journal of Nutrition that:
“Although high calcium intakes have long been recommended to prevent osteoporosis, there is little evidence that high calcium intakes effectively prevent fractures. Osteoporotic fractures are, like coronary artery disease, largely a disease of Western societies.”
Plant-based nutrients help bone density
Alkaline foods can be generalized as whole plant-based foods, because these foods provide alkalinity due to their natural content of minerals and micronutrients.
Illustrating this, studies have shown that increased intake of flavonoids – plant-based nutrients – have been shown to protect against the loss of bone density.
Researchers from the UK’s University of Anglia stated:
“Flavonoids may protect against osteoporosis by upregulating signaling pathways that promote osteoblast function, by reducing the effects of oxidative stress or chronic low-grade inflammation.”
Their comment regarding inflammation relates to other research showing that increased levels of pro-inflammatory cytokines and other inflammatory mediators have been seen among those with accelerated bone loss and the increased the risk of fracture.
Further to the point of the benefits of plant-based foods on bone health is the research showing that vitamin K an help reduce fractures. Vitamin K2 is a nutrient almost exclusive to plant-based foods.
We can add these to the other findings mentioned above regarding alkaline- and potassium-rich foods, together with the dismal results of calcium supplementation. We end up with a natural conclusion that nature provides a wealth of bone-building nutrients in the plant kingdom.
And if you feel you are deficient in calcium, plant-based sources of calcium include broccoli and citrus – and coral calcium is a source that also provides a balanced array of trace and macro minerals.
Osteoporosis linked to inflammation
Furthermore, we find that bone loss is linked to excess inflammation.
In 2005, researchers from Korea’s University of Ulsan College of Medicine (Koh et al. 2005) found that increased levels of circulating serum high sensitivity C-reactive protein (hsCRP) levels were linked to lower bone mineral density levels among otherwise healthy pre- and postmenopausal women. The research tested 3,662 premenopausal and 1,031 postmenopausal women.
They found that women with osteopenia and osteoporosis had 54% and 35% higher hsCRP levels, respectively. They also had significantly higher total alkaline phosphatase (ALP) levels – another marker for systemic inflammation. The researchers concluded:
“These findings suggest that subclinical systemic inflammation may be associated with bone turnover rate and bone mass in healthy women.”
In 2001, researchers from the UK’s University of Aberdeen Medical School found that the nitric oxide synthase pathway was activated in inflammation-induced osteoporosis. This research team found two years earlier that those with osteoporosis had 344% higher nitric oxide levels, and those higher levels were associated with 64% lower bone density than their control group. (Armour 1999)
Researchers from Stanford University found in their research that osteoporosis and inflammation was linked by “aging, menopause, reflex sympathetic dystrophy, HIV, pregnancy, transplantation, and steroid administration.” The research concluded:
“Osteoporosis may result from disequilibrium between structural demand for key minerals and their biologic demand during maladaptive states of inflammation.”
Medical researchers from The Netherlands’ University of Groningen (Arends et al. 2011) tested 128 osteoporosis patients with complications of ankylosing spondylitis. They found that those with the least bone densities shared higher inflammatory markers and lower vitamin D levels. They concluded, “This study indicates that increased bone turnover, inflammation, and low vitamin D levels are important in the pathophysiology of AS-related osteoporosis.”
Exercise and osteoporosis
The issue of inflammation brings us to exercise. Weight-bearing exercise and aerobic exercise in general has been linked to increased bone density and reduced fractures in a number of studies. Exercise is not only a way to strengthen the skeleton through weight bearing: It is also a means to reduce inflammation associated with bone loss.
REFERENCES:
Tai V, Leung W, Grey A, Reid IR, Bolland MJ. Calcium intake and bone mineral density: systematic review and meta-analysis. BMJ. 2015 Sep 29;351:h4183. doi: 10.1136/bmj.h4183.
Bolland MJ, Barber PA, Doughty RN, Mason B, Horne A, Ames R, Gamble GD, Grey A, Reid IR. Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial. BMJ. 2008 Feb 2;336(7638):262-6. doi: 10.1136/bmj.39440.525752.BE.
Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011 Apr 19;342:d2040. doi: 10.1136/bmj.d2040.
Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, Bassford T, Beresford SA, Black HR, Blanchette P, Bonds DE, Brunner RL, Brzyski RG, Caan B, Cauley JA, Chlebowski RT, Cummings SR, Granek I, Hays J, Heiss G, Hendrix SL, Howard BV, Hsia J, Hubbell FA, Johnson KC, Judd H, Kotchen JM, Kuller LH, Langer RD, Lasser NL, Limacher MC, Ludlam S, Manson JE, Margolis KL, McGowan J, Ockene JK, O’Sullivan MJ, Phillips L, Prentice RL, Sarto GE, Stefanick ML, Van Horn L, Wactawski-Wende J, Whitlock E, Anderson GL, Assaf AR, Barad D; Women’s Health Initiative Investigators. Calcium plus vitamin D supplementation and fractures. N Engl J Med. 2006 Feb 16;354(7):669-83.
Egger, M., G. Davey Smith, M. Schneider, C. Minder (1997), Bias in meta-analysis detected by a simple, graphical test British Medical Journal 315: 629-634.
Sterne, J.A.C., B.J. Becker, M. Egger (2005), The funnel plot. S. 75-98 in: H.R. Rothstein, A.J. Sutton, M. Borenstein (Hrsg.), Publication Bias in Meta-Analysis. Prevention, Assessment and Adjustments, The Atrium, Southern Gate, Chichester: John Wiley & Sons, Ltd.
Bolland MJ, Leung W, Tai V, Bastin S, Gamble GD, Grey A, Reid IR. Calcium intake and risk of fracture: systematic review. BMJ. 2015 Sep 29;351:h4580. doi: 10.1136/bmj.h4580.
Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, et al. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med2006;354:669-83.
Reid IR, Bolland MJ, Grey A. Effects of vitamin D supplements on bone mineral density: a systematic review and meta-analysis. Lancet. 2014 Jan
11;383(9912):146-55. doi: 10.1016/S0140-6736(13)61647-5.
Hirota T, Hirota K. Bone and Nutrition. Nutritional management of osteoporosis. Clin Calcium. 2015 Jul;25(7):1049-55. doi: CliCa150710491055.
Kuwabara A, Tanaka K. Bone and Nutrition. The association of vitamin K intake and bone health. Clin Calcium. 2015 Jul;25(7):983-90. doi: CliCa1507983990. Review. Japanese. PubMed PMID: 26119310.
Riaudel T, Guillot P, De Decker L, Gouraud-Tanguy A, Pichierri S, Chevalet P, Aoudia VO, Maugars Y, Berrut G. Nutrition and osteoporosis in elderly. Geriatr Psychol Neuropsychiatr Vieil. 2011 Dec 1;9(4):399-408. PubMed PMID: 22182816.
Suzuki H, Kondo K. Chronic kidney disease in postmenopausal women. Hypertens Res. 2011 Sep 8. doi: 10.1038/hr.2011.155.
Ogawa S, Ouchi Y. [Inflammatory control on lifestyle-related diseases and bone metabolism]. Clin Calcium. 2011 May;21(5):697-701.
Lencel P, Magne D. Inflammaging: the driving force in osteoporosis? Med Hypotheses. 2011 Mar;76(3):317-21.
Nakamura K, Saito T, Kobayashi R, Oshiki R, Oyama M, Nishiwaki T, Nashimoto M, Tsuchiya Y. C-reactive protein predicts incident fracture in community-dwelling elderly Japanese women: the Muramatsu study. Osteoporos Int. 2011 Jul;22(7):2145-50.
Frassetto LA, Todd KM, Morris RC Jr, Sebastian A. Worldwide incidence of hip fracture in elderly women: relation to consumption of animal and vegetable foods. J Gerontol A Biol Sci Med Sci. 2000 Oct;55(10):M585-92.
Frassetto L, Morris RC Jr, Sellmeyer DE, Todd K, Sebastian A. Diet, evolution and aging–the pathophysiologic effects of the post-agricultural inversion of the potassium-to-sodium and base-to-chloride ratios in the human diet. Eur J Nutr. 2001 Oct;40(5):200-13.
Frassetto LA, Morris RC Jr, Sellmeyer DE, Sebastian A. Adverse effects of sodium chloride on bone in the aging human population resulting from habitual consumption of typical American diets. J Nutr. 2008 Feb;138(2):419S-422S.
Sellmeyer DE, Stone KL, Sebastian A, Cummings SR. A high ratio of dietary animal to vegetable protein increases the rate of bone loss and the risk of fracture in postmenopausal women. Study of Osteoporotic Fractures Research Group. Am J Clin Nutr. 2001 Jan;73(1):118-22.
Koh JM, Khang YH, Jung CH, Bae S, Kim DJ, Chung YE, Kim GS. Higher circulating hsCRP levels are associated with lower bone mineral density in healthy pre- and postmenopausal women: evidence for a link between systemic inflammation and osteoporosis. Osteoporos Int. 2005 Oct;16(10):1263-71.
Mundy GR. Osteoporosis and inflammation. Nutr Rev. 2007 Dec;65(12 Pt 2):S147-51.
Hegsted DM. Fractures, calcium, and the modern diet. Am J Clin Nutr. 2001 Nov;74(5):571-3.
Hegsted DM. Calcium and osteoporosis? Adv Nutr Res. 1994;9:119-28.
Hegsted DM. Relationships between nutrition in early life and late outcomes including osteoporosis. Prog Clin Biol Res. 1990;326:73-87.
Hegsted DM. Calcium and osteoporosis. J Nutr. 1986 Nov;116(11):2316-9.
Frassetto LA, Todd KM, Morris RC Jr, Sebastian A. Worldwide incidence of hip fracture in elderly women: relation to consumption of animal and vegetable foods. J Gerontol A Biol Sci Med Sci. 2000 Oct;55(10):M585-92.
Frassetto L, Morris RC Jr, Sellmeyer DE, Todd K, Sebastian A. Diet, evolution and aging–the pathophysiologic effects of the post-agricultural inversion of the potassium-to-sodium and base-to-chloride ratios in the human diet. Eur J Nutr. 2001 Oct;40(5):200-13.
Frassetto LA, Morris RC Jr, Sellmeyer DE, Sebastian A. Adverse effects of sodium chloride on bone in the aging human population resulting from habitual consumption of typical American diets. J Nutr. 2008 Feb;138(2):419S-422S.
Sellmeyer DE, Stone KL, Sebastian A, Cummings SR. A high ratio of dietary animal to vegetable protein increases the rate of bone loss and the risk of fracture in postmenopausal women. Study of Osteoporotic Fractures Research Group. Am J Clin Nutr. 2001 Jan;73(1):118-22.
Welch AA, Hardcastle AC. The effects of flavonoids on bone. Curr Osteoporos Rep. 2014 Jun;12(2):205-10. doi: 10.1007/s11914-014-0212-5
Armour KJ, Armour KE, van’t Hof RJ, Reid DM, Wei XQ, Liew FY, Ralston SH. Activation of the inducible nitric oxide synthase pathway contributes to inflammation-induced osteoporosis by suppressing bone formation and causing osteoblast apoptosis. Arthritis Rheum. 2001 Dec;44(12):2790-6.
Koh JM, Khang YH, Jung CH, Bae S, Kim DJ, Chung YE, Kim GS. Higher circulating hsCRP levels are associated with lower bone mineral density in healthy pre- and postmenopausal women: evidence for a link between systemic inflammation and osteoporosis. Osteoporos Int. 2005 Oct;16(10):1263-71.
Yun AJ, Lee PY. Maldaptation of the link between inflammation and bone turnover may be a key determinant of osteoporosis. Med Hypotheses. 2004;63(3):532-7.
Arends S, Spoorenberg A, Bruyn GA, Houtman PM, Leijsma MK, Kallenberg CG, Brouwer E, van der Veer E. The relation between bone mineral density, bone turnover markers, and vitamin D status in ankylosing spondylitis patients with active disease: a cross-sectional analysis. Osteoporos Int. 2011 May;22(5):1431-9.